Frozen Shoulder (Adhesive Capsulitis)
Frozen shoulder, also known as adhesive capsulitis, can be a confusing and often misunderstood shoulder condition. It causes persistent pain, increasing stiffness, and a gradual loss of shoulder movement that can significantly affect daily activities, sleep, and quality of life.
While frozen shoulder can be slow to resolve, it is a condition that almost always improves over time with the right guidance, stage-appropriate care, and patience.
This page provides a clear clinical overview of frozen shoulder, including what it is, why it happens, how it progresses, and what treatments are most effective at each stage.
What Is Frozen Shoulder?
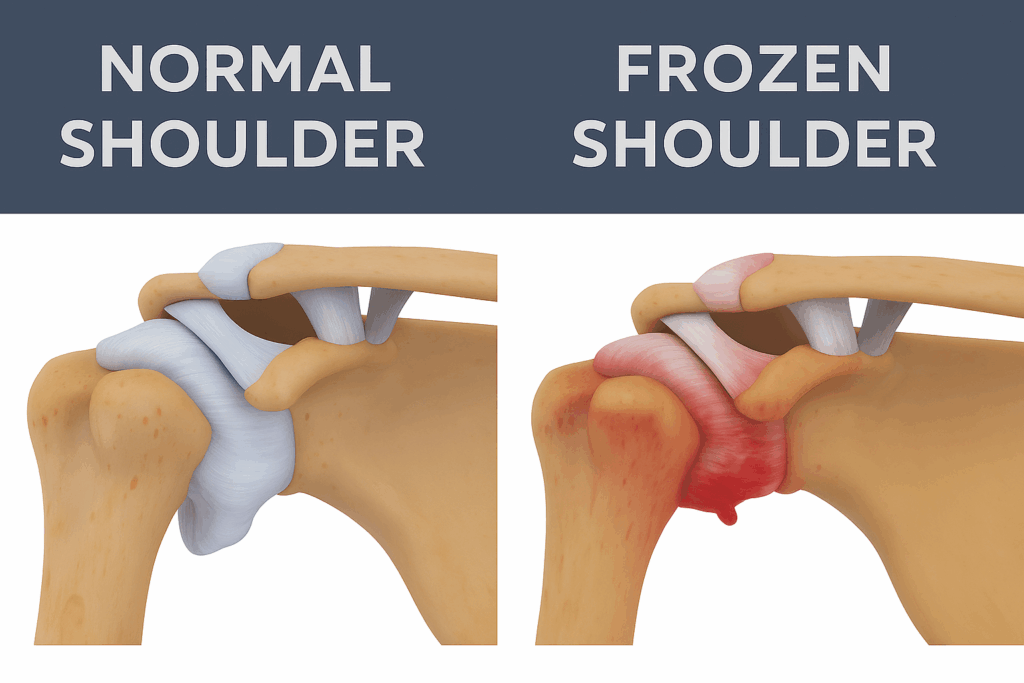
Frozen shoulder (adhesive capsulitis) occurs when the shoulder capsule becomes inflamed, thickened, and tight. This leads to:
- Pain (often significant)
- Progressive stiffness
- Difficulty sleeping
- The loss of movement can develop over weeks or months
It behaves differently from most other shoulder conditions, which is why accurate diagnosis and stage-specific treatment are so important.
Learn more here: What is Frozen Shoulder
Common Symptoms
Frozen shoulder symptoms include:
- Shoulder pain at rest and with movement
- Difficulty lifting the arm
- Restricted reach behind the back
- Night pain
- Gradual loss of motion over time
These symptoms can overlap with other conditions (e.g., bursitis, rotator cuff issues, impingement), so a proper assessment is essential.
See all frozen shoulder symptoms here.
Stages of Frozen Shoulder
Understanding how symptoms change over time can help you know what to expect.
In adhesive capsulitis, pain often peaks early (freezing phase), while stiffness may continue even after pain declines. The graph below illustrates this common pattern.
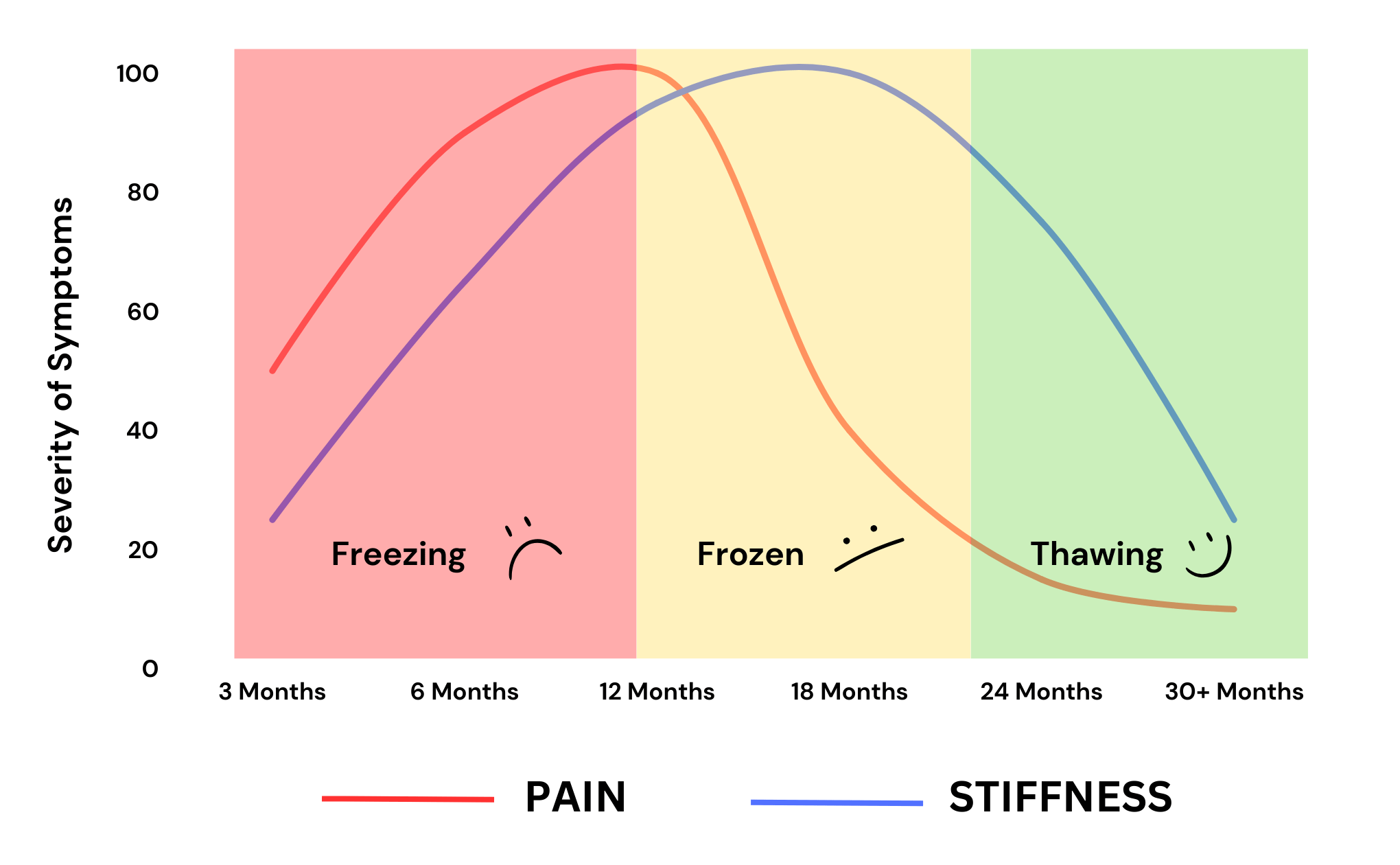
Frozen shoulder progresses through three main stages:
Freezing Stage (Pain-Dominant)
- Increasing shoulder pain
- Pain often worse at night
- Movement becomes progressively limited
- Typical duration: ~6 weeks to 12 months
Frozen Stage (Stiffness-Dominant)
- Pain may begin to settle
- Marked stiffness and restricted movement
- Daily activities remain difficult
- Typical duration: ~6 to 12 months
Thawing Stage (Recovery)
- Gradual improvement in movement
- Pain continues to ease
- Function slowly returns
- Typical duration: ~6 to 12 months
Each stage behaves differently and requires a different treatment approach.
Learn about the frozen shoulder stages in detail.
Why Does Frozen Shoulder Happen?
The exact cause of frozen shoulder is not always clear. It may develop without an obvious injury, or after a period of reduced shoulder movement.
Factors associated with a higher risk include:
- Age between 40 and 60 years
- Female sex (2x more likely than male)
- Diabetes (both type 1 and type 2)
- Thyroid disorders
- Prolonged shoulder immobility (after injury or surgery)
Frozen shoulder can occur in otherwise healthy people and does not mean you have done anything “wrong”.
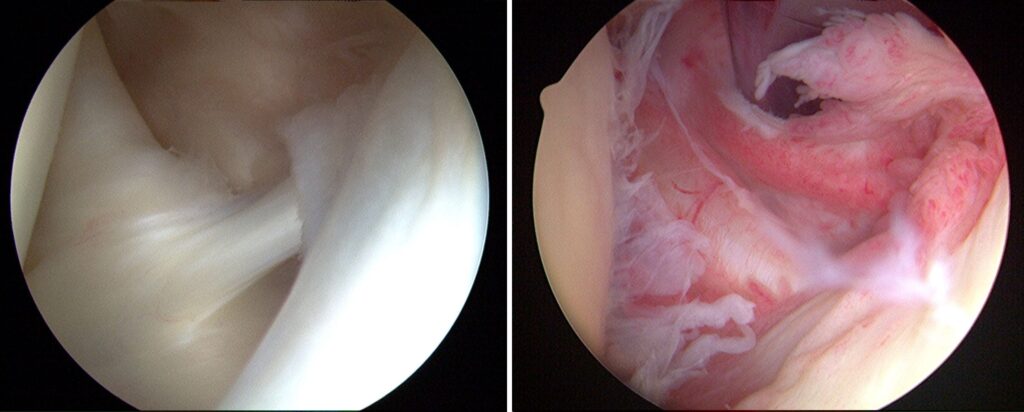
How is Frozen Shoulder Diagnosed?
Frozen shoulder is primarily a clinical diagnosis, based on your history and a physical examination.
Imaging such as X-ray or MRI may be used to rule out other causes of shoulder pain, but they do not diagnose frozen shoulder itself.
Other shoulder conditions — such as rotator cuff pathology, bursitis, or arthritis — can produce similar symptoms. A thorough assessment helps differentiate these and ensures appropriate management.
Treatment for Frozen Shoulder
The most effective treatment for frozen shoulder depends on the stage of the condition.
In general:
- Early stages focus on pain control and inflammation management
- Later stages focus on gentle, progressive movement and strength
- Overly aggressive treatment can delay recovery
Evidence-based treatments may include:
- Education and activity modification
- Physiotherapy tailored to the stage of the condition
- Corticosteroid injections (particularly early in the course)
- Time and graduated return to movement
You can explore Frozen Shoulder Treatment in more detail here.
Injection Options
A cortisone injection can be effective during the early pain-dominant stage, especially when performed into the glenohumeral joint under imaging guidance.
Learn which injections help for frozen shoulder and which don’t.
Exercises for Frozen Shoulder
Not all exercises are appropriate for every stage.
The best exercises depend on whether your shoulder is:
- Pain-dominant
- Stiffness-dominant
- Starting to recover
Doing the wrong exercises too early can flare symptoms, while doing too little later can slow progress.
View frozen shoulder exercises suited to each stage.
How Long Does Recovery Take?
Recovery from frozen shoulder is often slower than people expect. While symptoms can persist for many months, improvement does occur gradually.
Most people experience:
- Meaningful pain relief before full movement returns
- Slow but steady gains over time rather than sudden improvement
The goal of treatment is to:
- Reduce pain and flare-ups
- Maintain as much movement as possible
- Support recovery without aggravating the condition
Read more about how long frozen shoulder lasts
Frozen Shoulder FAQs
Common questions include:
- Should I stretch a frozen shoulder?
- How do I know what stage I’m in?
- Will it get better on its own?
- Do I need imaging?
- When should I see a physio?
See all Frozen Shoulder FAQs
Frozen Shoulder Self-Care Guide
For a deeper, step-by-step recovery plan — including exercises, pain management strategies, sleep tips, timelines, and stage-specific advice — explore our full Frozen Shoulder Treatment Guide.
When Should You Seek Help?
You should consider professional assessment if:
- Shoulder pain and stiffness persist beyond several weeks
- Night pain is severe or worsening
- Daily activities are becoming increasingly difficult
- You are unsure whether your symptoms are frozen shoulder or another condition
Early, stage-appropriate management can significantly improve comfort and reduce unnecessary frustration.
Expert Care for Frozen Shoulder in Perth
At Perth Shoulder Physio, frozen shoulder is a common condition we assess and treat. Our approach is based on:
- Accurate stage identification
- Evidence-based treatment strategies
- Clear education and expectation setting
- Individualised rehabilitation plans
If you’d like personalised guidance, you can book an appointment below.