Frozen Shoulder FAQs
Frozen shoulder can be confusing, painful, and frustrating — especially when symptoms don’t behave like a typical shoulder injury.
This page answers the most common frozen shoulder questions, including pain, stiffness, stages, exercises, injections, and recovery timelines, based on clinical experience treating frozen shoulder every week.
If you’re unsure whether you have frozen shoulder, what stage you’re in, or what treatment is appropriate, these answers will help you understand what’s happening and what to do next.
👉 For a more detailed, step-by-step framework (including less common questions), see our:
What is frozen shoulder?
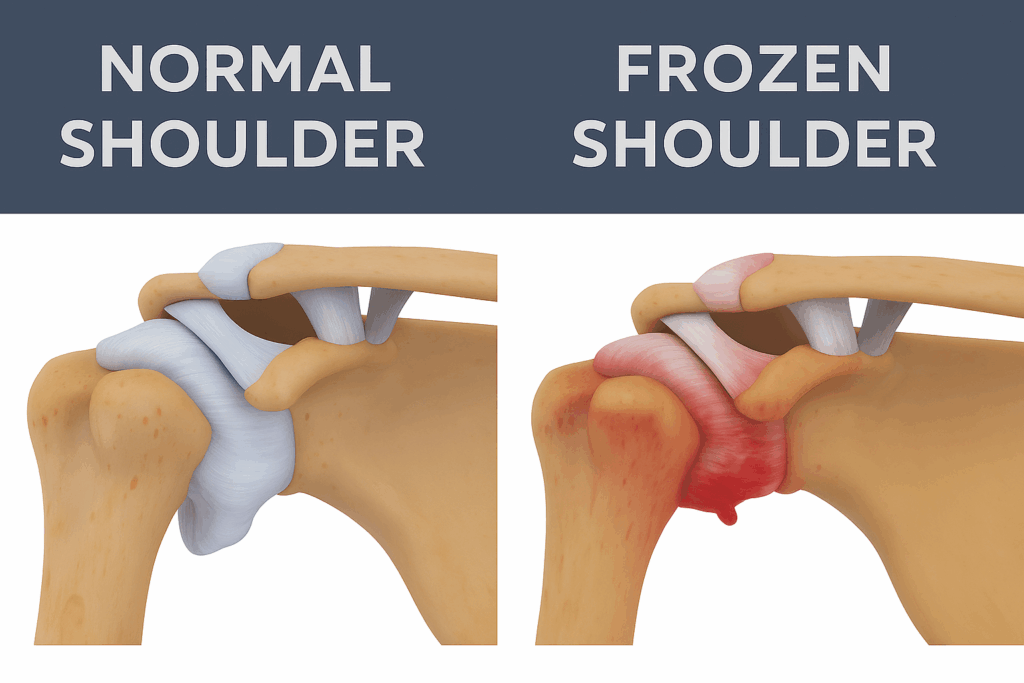
Frozen shoulder, also known as adhesive capsulitis, is a condition where the shoulder joint becomes painful and progressively stiff due to inflammation and thickening of the joint capsule.
It typically develops gradually and can significantly limit daily activities such as dressing, reaching, and sleeping comfortably.
What causes frozen shoulder?
In many cases, frozen shoulder develops without a clear cause.
Known risk factors include:
- Diabetes
- Thyroid conditions
- Prolonged shoulder immobilisation
- Recent shoulder injury or surgery
- Age (most common between 40–65 years)
What are the stages of frozen shoulder?
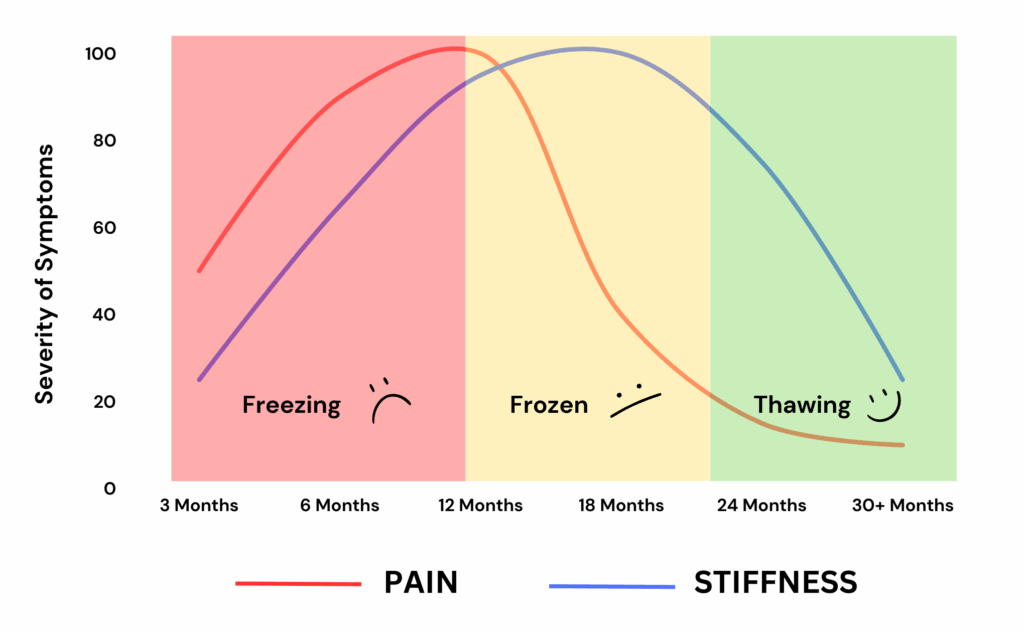
Frozen shoulder usually progresses through three overlapping stages:
- Freezing stage – increasing pain and night pain
- Frozen stage – pain settles, stiffness dominates
- Thawing stage – gradual return of movement
👉 Read more on our Frozen Shoulder Stages page.
How long does frozen shoulder last?
Frozen shoulder commonly lasts 12–36 months, though this varies widely.
Some people recover faster, particularly when the condition is recognised early and managed appropriately. Others may experience symptoms for longer.
👉 See typical timeframes on our Frozen Shoulder Recovery Timeline page.
Does frozen shoulder go away on its own?
In many cases, frozen shoulder does improve over time.
However, recovery is not always complete, and symptoms may persist without appropriate management.
Early diagnosis, education, and symptom control can make the recovery process more manageable and less disruptive.
Should I keep exercising with frozen shoulder?
Yes — but only the right exercises at the right time.
Aggressive stretching or strengthening too early can worsen pain, especially during the freezing stage. Exercises should be matched to the current stage of the condition.
👉 See our full guide to Frozen Shoulder Exercises.
Can exercises make frozen shoulder worse?
Yes.
Doing exercises that are:
- Too aggressive
- Too frequent
- Not appropriate for your stage
can increase pain and delay recovery.
Pain that worsens at night or lasts more than 24 hours after exercise is often a sign you’re doing too much.
Are injections helpful for frozen shoulder?
Injections can be very helpful — particularly early in the freezing stage when pain is severe or escalating.
Corticosteroid injections may reduce inflammation, improve sleep, and allow earlier, more comfortable movement. They work best when combined with appropriate rehabilitation.
👉 Learn more on our Frozen Shoulder Injections page.
What is the difference between cortisone injection and hydrodilatation?
- Cortisone injections primarily target pain and inflammation
- Hydrodilatation aims to stretch the joint capsule to improve movement
They may be considered at different stages, depending on whether pain or stiffness is the main issue.
Is frozen shoulder the same as rotator cuff injury?
No.
Frozen shoulder is a capsular condition that restricts both active and passive movement.
Rotator cuff injuries primarily affect strength and active movement, while passive movement is often preserved.
Why is frozen shoulder pain worse at night?
Night pain is common due to:
- Inflammation inside the joint
- Difficulty finding a comfortable sleeping position
- Reduced movement overnight
This is especially common during the freezing stage.
Should I get imaging (MRI or ultrasound)?
Imaging is not always required to diagnose frozen shoulder. Diagnosis is usually based on history and physical examination.
Imaging may be used to:
- Exclude other causes of shoulder pain
- Guide injections if required
When should I see a physiotherapist?
You should seek assessment if:
- Pain is worsening
- Night pain is persistent
- Movement is progressively reducing
- You’re unsure which exercises are safe
A physiotherapist experienced with frozen shoulder can help guide management and reduce unnecessary flare-ups.
Can frozen shoulder come back?
It is uncommon for frozen shoulder to recur in the same shoulder, but it can occur in the opposite shoulder, particularly in people with diabetes.
Are there questions not covered here?
Yes.
Frozen shoulder raises many stage-specific and individual questions, including:
- How to exercise after an injection
- What movements to avoid at work or sport
- How to manage flare-ups
- Which treatments don’t help — or may make things worse
These are covered in more detail in our Frozen Shoulder Treatment Guide.