Frozen Shoulder Injections
Frozen shoulder injections can be an effective pain-relief and symptom-modifying tool, particularly when used early in the condition.
While injections are not a cure on their own, the right injection at the right time may help:
- Settle joint inflammation
- Reduce escalating pain
- Limit how severe frozen shoulder becomes
On this page, we explain:
- When injections are most helpful
- What type of injection is used
- What injections can and cannot do
- How injections fit into a complete frozen shoulder recovery plan
What Injection is Used for Frozen Shoulder?
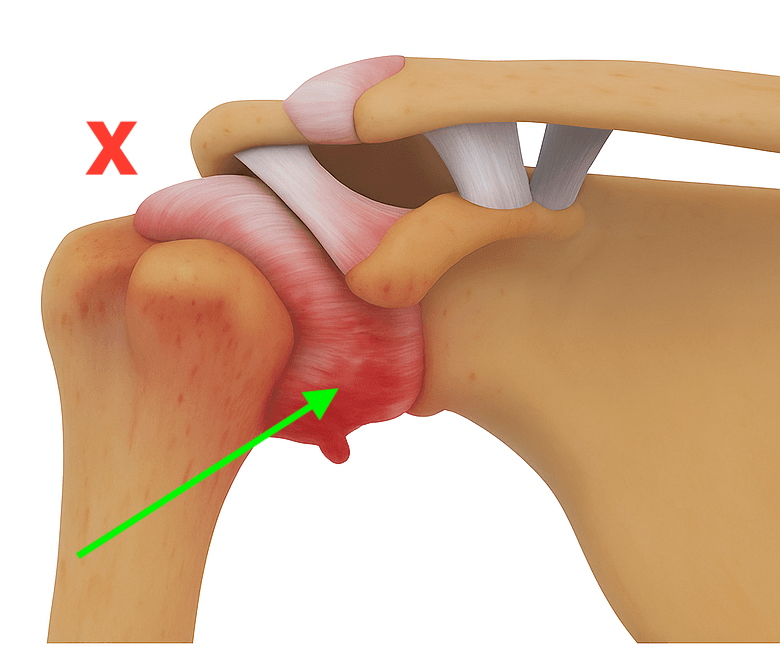
The most commonly used injection for frozen shoulder is a corticosteroid (cortisone) injection, delivered directly into the shoulder joint (glenohumeral joint).
In most cases, this injection is:
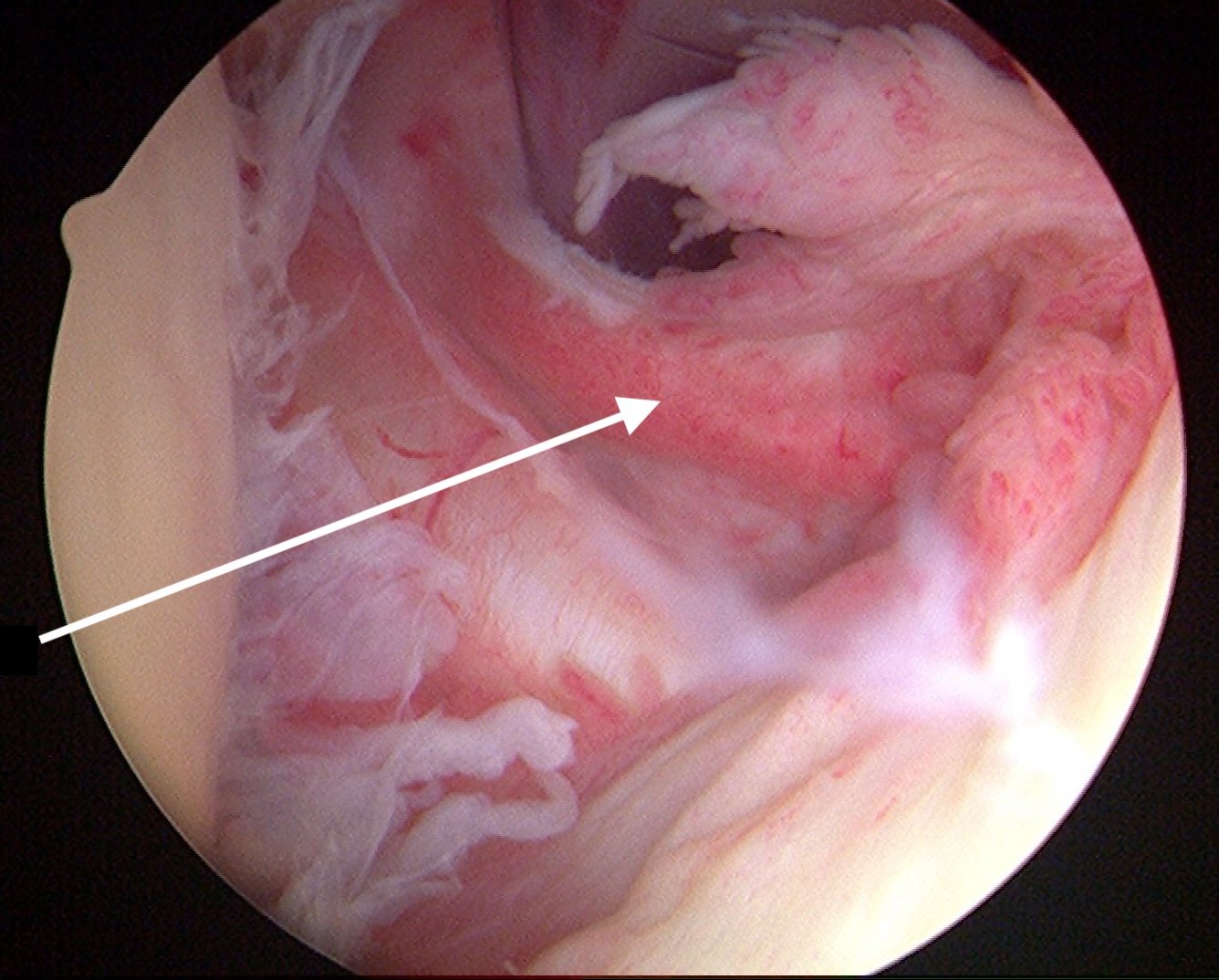
- CT-guided or ultrasound-guided for accuracy
- Combined with a local anaesthetic
- Performed by a radiologist, sports physician, or specialist
Accurate placement into the joint is important, as this is where inflammation driving frozen shoulder occurs.
What Does a Frozen Shoulder Injection Do?
A corticosteroid injection aims to:
- Reduce inflammation inside the shoulder joint
- Decrease pain, particularly night pain
- Improve tolerance to daily movement and exercise
When used early, reducing inflammation may help prevent ongoing pain-driven guarding and protective stiffness, which can otherwise contribute to worsening symptoms over time.
When Are Injections Most Helpful?
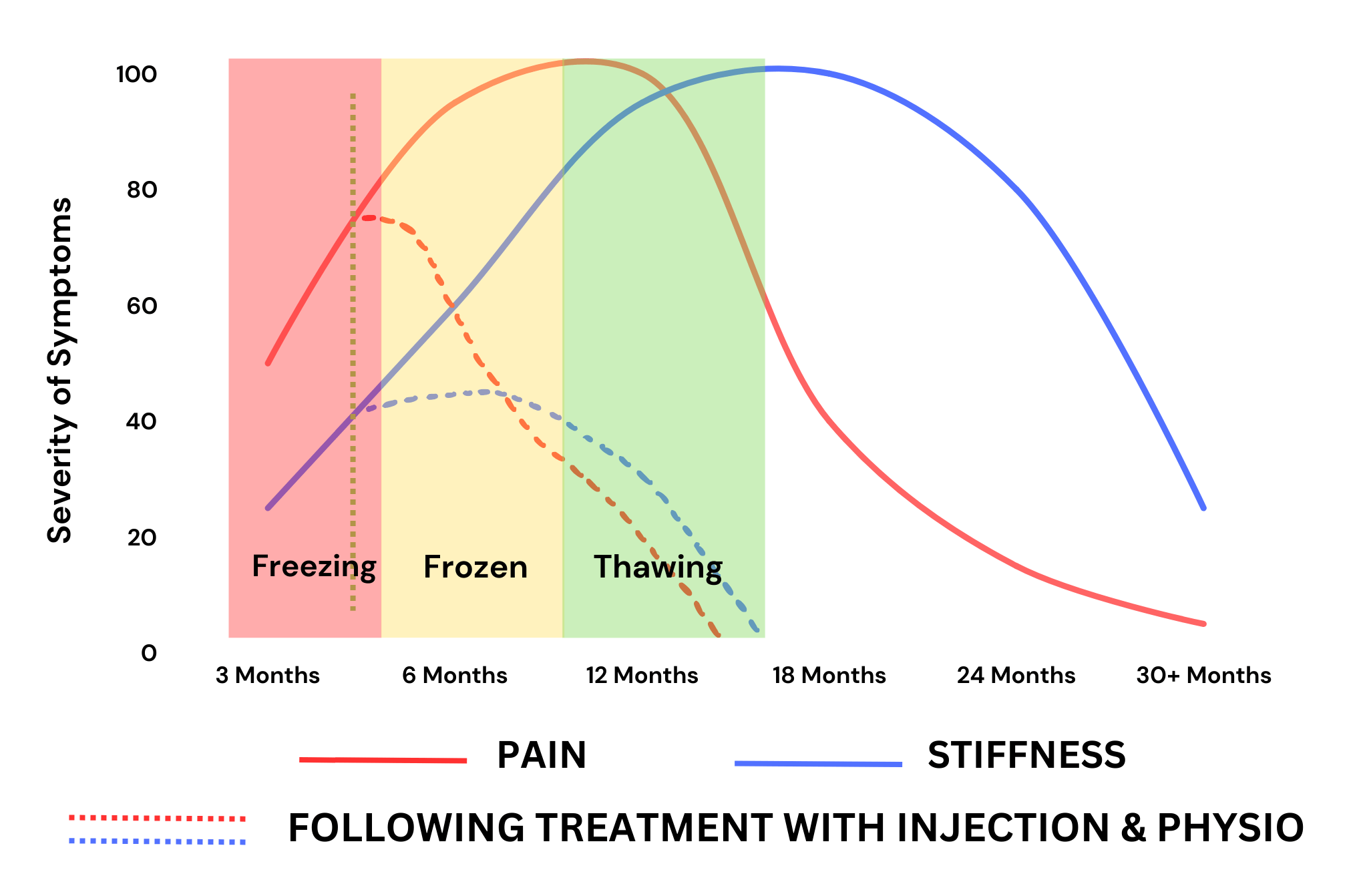
Frozen shoulder injections are most effective during the early, pain-dominant (freezing) stage, when inflammation inside the joint is highest.
When used at this stage, an injection may:
- Settle severe or worsening pain
- Improve sleep by reducing night pain
- Allow earlier and more comfortable movement
- Reduce ongoing joint irritation that can drive further stiffness
In some cases, early pain control can help limit how aggressive the condition becomes, particularly when combined with stage-appropriate exercises and education.
As frozen shoulder progresses into later stages, injections may still provide pain relief, but their ability to influence the overall course of the condition is often reduced.
Cortisone Injection vs Hydrodilatation (Hydrodistension)
Two injection-based treatments are commonly discussed for frozen shoulder: corticosteroid injections and hydrodilatation (also called hydrodistension).
While both aim to reduce symptoms, they work in different ways and may be more suitable at different stages of the condition.
Cortisone Injection
A cortisone injection targets inflammation inside the shoulder joint.
Primary role:
- Reduce pain and inflammation
- Improve sleep and comfort
- Allow better tolerance to movement and exercise
Most helpful when:
- Pain is severe or worsening
- Night pain is prominent
- The condition is in the freezing (early) stage
When used early, cortisone injections may help limit escalating pain and secondary stiffness, particularly when combined with appropriate exercises.
Hydrodilatation (Hydrodistension)
Hydrodilatation involves injecting a larger volume of fluid into the shoulder joint to gently stretch the joint capsule. It may include saline, local anaesthetic, and corticosteroid.
Primary role:
- Improve shoulder movement
- Reduce capsular tightness
- Assist stiffness-dominant presentations
May be considered when:
- Stiffness is the main limitation
- Pain is more settled
- Progress has plateaued despite rehabilitation
Hydrodilatation is typically used later than a simple cortisone injection, although individual responses vary.
Which Is Better for Frozen Shoulder?
There is no single “best” injection for everyone.
In general:
- Cortisone injections may be more helpful for pain-dominant, early-stage frozen shoulder
- Hydrodilatation may be considered when stiffness is the primary issue, particularly if recovery has stalled
Both treatments work best when they are part of a broader management plan, rather than used in isolation.
Important:
Neither cortisone injections nor hydrodilatation guarantee faster recovery. Timing, stage, and follow-up rehabilitation play a major role in outcomes.
The most appropriate injection — and timing — depends on your stage of frozen shoulder, pain levels, and response to treatment.
👉 View the Frozen Shoulder Treatment Guide for a clearer framework around injections and recovery.
How Long Does a Frozen Shoulder Injection Last?
Response to injection varies between individuals.
Most people experience:
- Pain relief within days to a week
- Reduced symptoms for months
- Enough comfort to progress exercises meaningfully
Others may only notice:
- Partial or short-term improvement
- Minimal response
Effectiveness depends on timing, stage of frozen shoulder, and individual factors.
Do Injections Replace Physiotherapy or Exercises?
No.
Injections work best when they are used to support a broader treatment plan, not replace it. This typically includes:
- Stage-appropriate exercises
- Education about what to expect
- Gradual return to normal movement
- Ongoing monitoring of symptoms
Without the right exercises and guidance, pain relief from an injection may be short-lived.
👉 Learn more about comprehensive management on our Frozen Shoulder Treatment page.
Should Everyone With Frozen Shoulder Get an Injection?
No.
Many people recover without injections, particularly when the condition is managed appropriately.
However, for people in the freezing stage with escalating pain, an injection may:
- Help prevent symptoms from worsening further
- Reduce reliance on pain medication
- Allow earlier and more comfortable movement
Injections are a tool, not a requirement. The decision should always be individualised.
Clinical overview of adhesive capsulitis – AAOS
Want a Clearer Plan Around Injections and Recovery?
Our Frozen Shoulder Treatment Guide explains:
- When injections are most likely to help
- How injections fit into each stage of recovery
- How to modify exercises after an injection
- Other injections that may help
- Common mistakes that delay recovery
- Injections that don't help of make things worse